
The Hidden Cost of Inefficiency in Healthcare
Three weeks to see a specialist. Two hours on hold with insurance. A billing error that takes six months to resolve.
If you’ve navigated the American healthcare system lately, you know these aren’t edge cases—they’re the norm. Behind every frustrating delay sits a deeper dysfunction: the U.S. healthcare system burns roughly $450 billion annually on administrative overhead. That’s nearly a third of all healthcare spending, which means for every nurse at a patient’s bedside, there’s roughly another person drowning in paperwork, chasing down prior authorizations, or redialing insurance hotlines.
The irony is sharp. While fintech startups automate loan approvals in minutes and logistics companies track shipments in real time, many hospitals still rely on fax machines and manual phone trees. It’s not for lack of trying—healthcare is just brutally complex. Regulatory landmines, interoperability nightmares, and the high stakes of medical data have made the industry notoriously resistant to change.
But something’s shifting. Prosper AI, a healthcare automation startup founded in 2023, just closed a $5 million seed round to attack this problem with a deceptively simple tool: voice AI that actually works in medical settings. Not a chatbot. Not a pilot program. A deployed system already handling calls for hundreds of thousands of providers, including Providence-affiliated hospitals and Fortune 50 pharma companies.
The company’s trajectory suggests the technology has finally caught up to the promise. Revenue quadrupled in three months. That’s not hype—that’s traction.
Why Healthcare Automation Has Been So Hard
Here’s the thing about healthcare AI: it’s easy to demo, hard to deploy.
A voice assistant that books restaurant reservations is impressive. One that navigates a multi-layered insurance verification call—without hanging up on a patient or violating HIPAA—is an entirely different beast. The workflows are labyrinthine. The stakes are existential. And the tolerance for error is essentially zero.
That’s why so many healthcare AI projects stall in the pilot phase. Accuracy isn’t enough if latency makes conversations feel robotic. Compliance isn’t enough if the system can’t integrate with legacy EHR software. And cost savings don’t matter if staff won’t trust the tool.
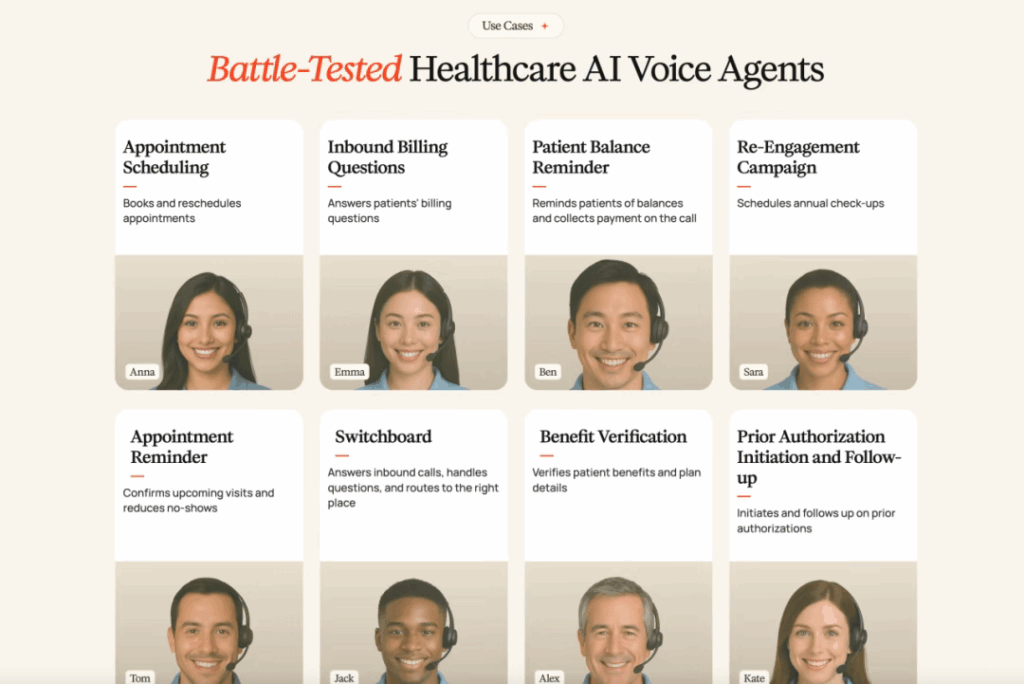
Prosper AI’s approach acknowledges these realities upfront. The company doesn’t try to replace clinicians or overhaul entire hospital systems. Instead, it targets the repetitive, time-consuming administrative calls that burn out front-desk staff and delay patient care—appointment scheduling, insurance benefit verification, claim follow-ups. Unglamorous work. Enormous impact.
Inside the Technology
Prosper AI’s voice agents aren’t built on a single AI model—they’re orchestrated systems combining OpenAI, Google, and proprietary layers to handle the chaos of real-world medical calls.
The technical benchmarks are striking:
- Sub-0.5-second latency for natural voice responses
- 99% accuracy navigating insurance phone menus
- Under two hours to complete benefit verification checks
- End-to-end automation—from call initiation to EHR updates
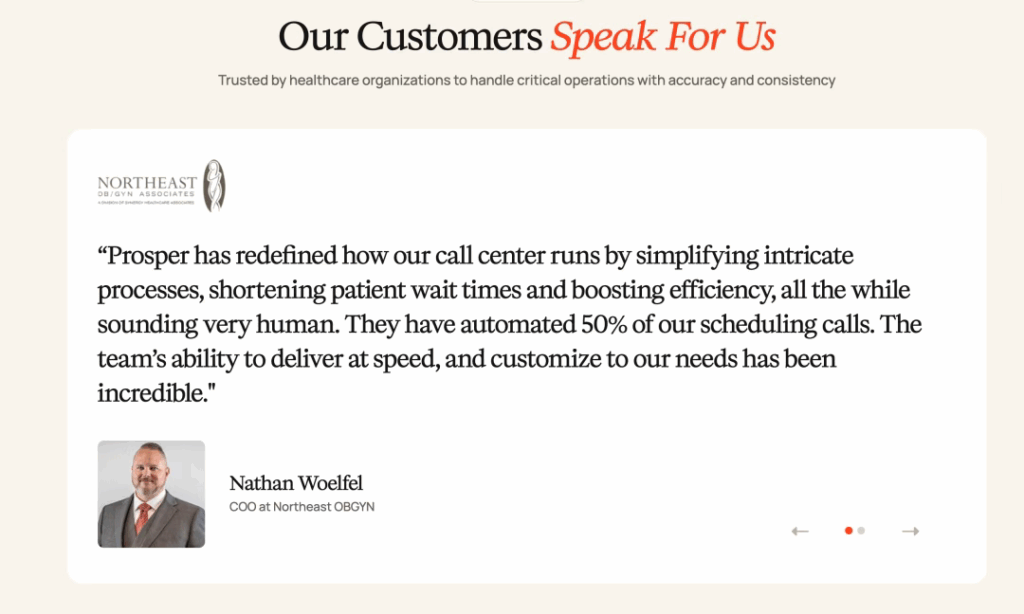
But the real innovation isn’t speed or accuracy in isolation. It’s building a system reliable enough that hospitals will let it run unsupervised. At Synergy Healthcare Associates, Prosper’s AI now handles over half of front-desk calls. That’s not a trial. That’s operational.
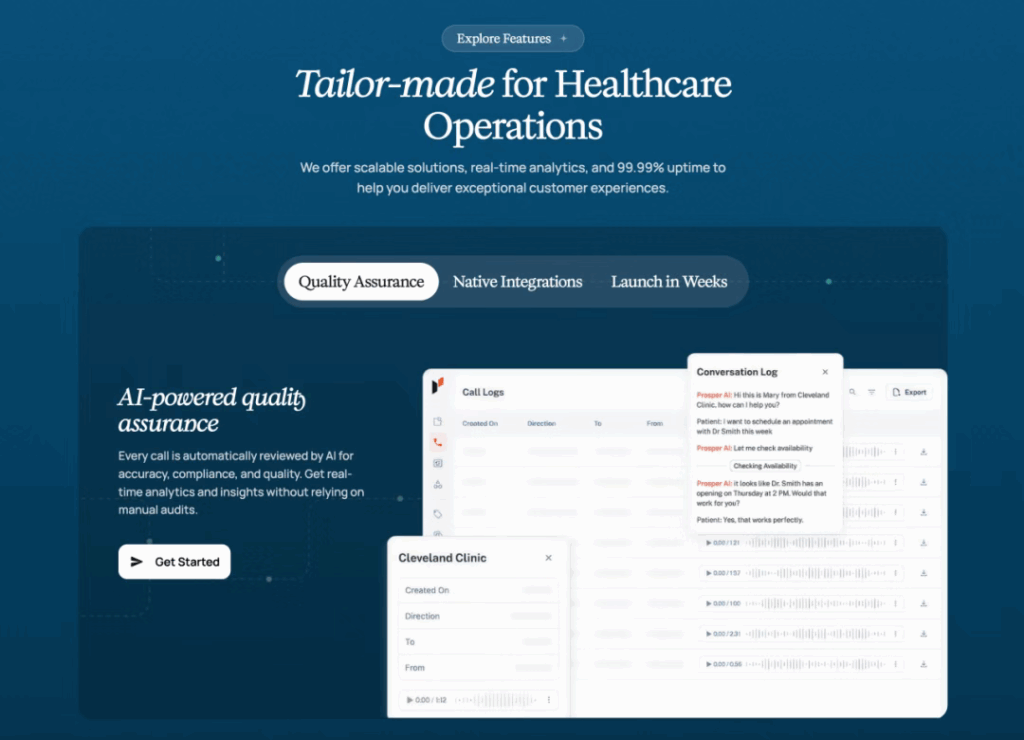
The technology works because it’s designed for healthcare’s specific friction points. Generic voice recognition breaks down when confronted with medical terminology, insurance jargon, and the endless edge cases of billing codes. Prosper’s system is trained on those exact scenarios—the frustrated patient calling about a denied claim, the insurer’s hold music, the EHR field that needs updating after a benefit check.
It’s automation that feels human because it anticipates the mess.
The Math of Administrative Waste
Let’s zoom out. Roughly one-third of U.S. healthcare workers are employed in administrative roles. That’s not a typo. For every three people working in American healthcare, one is managing paperwork, not patients.
Prosper AI’s value proposition is straightforward: automate the repetitive stuff, redeploy the humans to higher-value work. The company’s clients report tangible improvements—shorter patient wait times, faster insurance approvals, lower overhead costs. At scale, those efficiencies compound.
Consider what happens when an insurance verification that previously took a staff member two days of phone tag gets completed in 90 minutes by an AI agent. Multiply that across thousands of calls per month. The labor savings are significant, but the real win is operational velocity—fewer appointment cancellations due to insurance confusion, faster patient onboarding, less staff burnout from soul-crushing phone work.
Automation also cuts errors. Each manual handoff—transcribing a benefits summary, updating a patient record, transferring a call—introduces risk. Eliminating those steps means fewer billing mistakes, fewer denied claims, fewer angry patients.
The Founders’ Origin Story
Xavier de Gracia and Josep Mingot met at Harvard and MIT, where they saw firsthand how much organizational energy gets wasted on low-value tasks. Xavier had spent time in enterprise operations at Bain and a public tech firm, watching teams drown in process. Josep brought deep expertise in AI and insurance—two domains that intersect awkwardly in healthcare.
Their founding thesis was simple: healthcare can’t afford to keep throwing human labor at administrative sludge. The mission isn’t just efficiency for its own sake—it’s making healthcare genuinely more affordable by eliminating waste at the system level.
What’s notable is how quickly they’ve gained traction in an industry famous for moving slowly. Since launching in 2023, Prosper AI has signed contracts with major health systems and pharmaceutical companies. That kind of adoption suggests they’re solving a pain point urgent enough to overcome healthcare’s institutional inertia.
Why Investors Are Betting Big
Prosper AI’s seed round was led by Emergence Capital, with participation from Y Combinator, CRV, and Company Ventures. The pitch is compelling: a $450 billion problem, AI technology that’s finally mature enough to handle it, and early proof points showing rapid revenue growth.
Investors also see structural tailwinds. Post-pandemic, hospitals are under immense financial pressure. Labor costs are rising. Staffing shortages are chronic. Payers are scrutinizing every line item. Meanwhile, AI models have quietly gotten good enough to handle sensitive, regulated workflows—something that wasn’t true even two years ago.
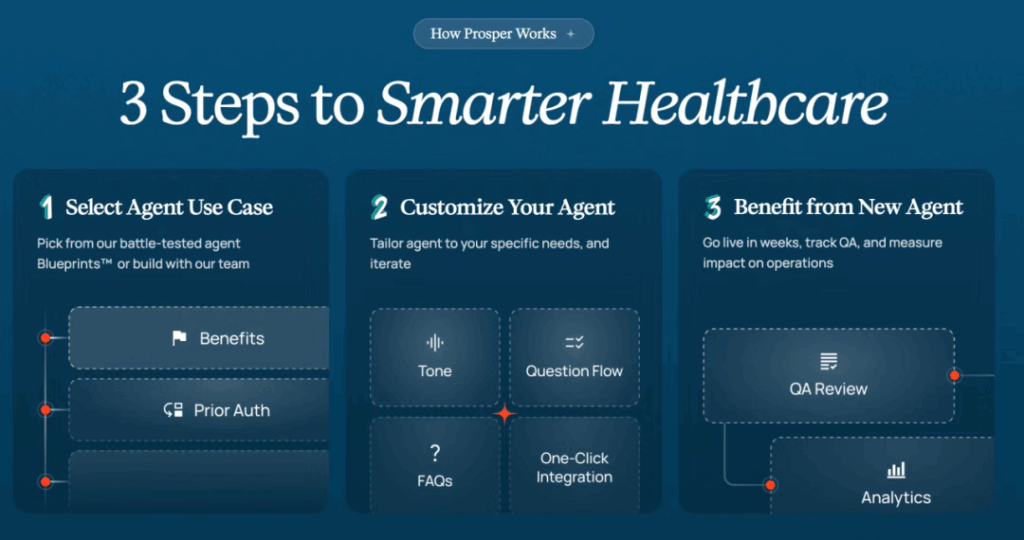
Prosper’s defensibility comes from domain depth. This isn’t a horizontal AI platform trying to serve every industry. It’s purpose-built for healthcare’s idiosyncrasies—HIPAA compliance, EHR integration, insurance protocols. That specialization creates both technical moats and customer stickiness.
Real-World Results
The numbers tell the story. Across Prosper AI’s client base:
- 50-70% of inbound calls are handled by AI agents
- 99% accuracy navigating insurance voice menus
- Hours, not days, for benefit verification
Hospitals report measurable improvements in patient satisfaction, employee morale, and cost metrics—the trifecta any CFO wants to see. The AI runs 24/7 without fatigue, maintains consistent quality, and scales without adding headcount.
One client noted that front-desk staff, freed from endless phone loops, could finally focus on complex patient issues requiring human judgment. That’s the promise of automation done right—not replacing people, but letting them do the work only they can do.
What This Means for Healthcare’s Future
If Prosper AI’s model scales, the implications are profound. Redirecting even a fraction of that $450 billion from administrative overhead to clinical care could mean more nurses, better equipment, shorter wait times, expanded access.
For patients, it translates to fewer friction points—easier scheduling, faster insurance approvals, less time navigating bureaucratic mazes. For healthcare workers, it means less burnout from soul-crushing busywork.
And the model isn’t U.S.-specific. Asia, where healthcare costs and staffing shortages are escalating, could leapfrog directly to AI-first administration. Prosper’s playbook—voice automation, EHR integration, workflow orchestration—is replicable anywhere the administrative burden outweighs the clinical capacity.
The Road Ahead
Of course, challenges remain. Data privacy is non-negotiable in healthcare. HIPAA compliance is table stakes, but patient trust is harder to earn. Competitors like SuperDial, Infinitus Systems, and Suki are attacking similar problems, each with different technical approaches.
Prosper will need to keep innovating—expanding beyond voice into API automation, deeper EHR operations, perhaps even clinical workflows. The technology is proven, but the market is still being defined.
What’s clear is that AI has crossed the chasm from experimental to operational. Healthcare automation isn’t a future trend waiting to arrive. It’s already here, rewriting the economics of medical administration one phone call at a time.
The question isn’t whether AI will transform healthcare—it’s how fast, and who will lead.
Tags:
Subscribe To Get Update Latest Blog Post
[mc4wp_form id=664]


Leave Your Comment: